New study may inform chemotherapy approaches for breast cancer
A new Virginia Tech study found platinum-based chemotherapy, although effective, may be improved by blocking its effects on the lymphatic system
Breast cancer is the second-leading cause of cancer death among women in America, according to the Centers for Disease Control and Prevention. Platinum-based chemotherapy drugs are regularly prescribed to treat the cancer, but in a first-of-its-kind finding, Virginia Tech researchers have found these drugs may activate the patient’s lymphatic system and help tumor cells to spread to healthy parts of the body.
A new study, published in Frontiers in Oncology, by a multi-institutional team of researchers led by Jennifer Munson, associate professor at the Fralin Biomedical Research Institute at VTC, helps explain how platinum-based chemotherapies might be made more effective if the changes to the lymphatic system caused by the chemotherapy can be blocked or even reversed by an additional therapy.
Because the lymphatic system contributes to the body’s immune response, it’s possible that growth of the lymphatics has a positive effect on fighting tumors, an aspect the study did not explore. More research is needed, said Munson, who is also an associate professor in Virginia Tech’s Department of Biomedical Engineering and Mechanics and co-director of the Virginia Tech Cancer Research Alliance.
She said the findings highlight the incomplete understanding of the impact of chemotherapy on tissues in the body and that more study is crucial to advancing the treatment of aggressive breast cancers.
“These chemotherapy drugs do work,” Munson said. “They kill tumor cells. What’s needed is a combination of the right co-treatments and the right dosing strategies for patients.”
Munson’s team focused on triple-negative breast cancers — tumors that lack receptors for the three most common and effective breast cancer treatments, leaving doctors to rely on surgeries, radiation, and chemotherapy as front-line treatments.
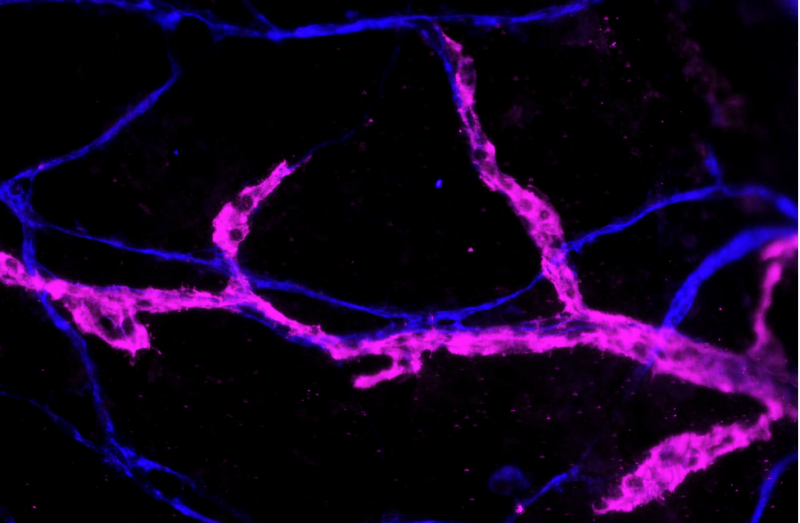
Studying tissue-engineered and animal models, as well as tissue samples from human patients, Munson and her research team found the chemotherapy drugs triggered systemic growth and activation of lymphatic vessels throughout the body, including sites vulnerable to the spread of cancer cells such as the lungs.
After treatments, remaining therapy drugs drain via the lymphatic system, but little was known about the effect of the drugs on the system. Lymphatic vessel cell proliferation is associated with the growth and spread of cancer.
“If you have more lymphatics, it will actually kind of prime your body for metastatic spread,” Munson said. “While this can sound like bad news, it’s important to know in order to make informed decisions about treating patients with breast cancer. By knowing this, physicians can better formulate treatments for their patients to kill tumors without these side effects.”
Munson’s study offers a solution: Treating patients who receive these chemotherapies with a drug that inhibits a protein called VEGFR3, which is important to the growth and proliferation of lymphatic vessels.
The research found the chemotherapy-induced growth of the vessels depended on the protein. Alternating the chemotherapy with the protein-inhibiting drug prevented the side effect and even reversed it.
Scientists from Virginia Tech, the University of Virginia, the Lerner Research Institute, Brown University, and Women & Infants Hospital of Rhode Island collaborated on the research.
Funding for the research was provided by the Kincaid Foundation and the University of Virginia Cancer Center; the Marty Whitlow Fund; the National Eye Institute; National Cancer Institute; Susan G. Komen Career Catalyst award; the University of Virginia Cancer Center; the National Institute of General Medical Sciences; the National Institute of Allergy and Infectious Diseases; the National Cancer Institute, and the Fralin Biomedical Research Institute.





