Researchers develop miniature optical fiber treatment device for more effective cancer immunotherapy
Cancer immunotherapy, one of the most important and promising therapies for cancer treatments, is being used by oncologists to treat patients suffering from many different cancers including breast, cervical, colon, stomach, and skin.
“However, an obstacle to achieving more than moderate success,” said Rong Tong, assistant professor in the Department of Chemical Engineering, “is none of the current delivery strategies can sustainably supply drugs that can, over the course of a few weeks, adjust the drug dose either to lower systemic toxicities or to augment therapeutic response.”
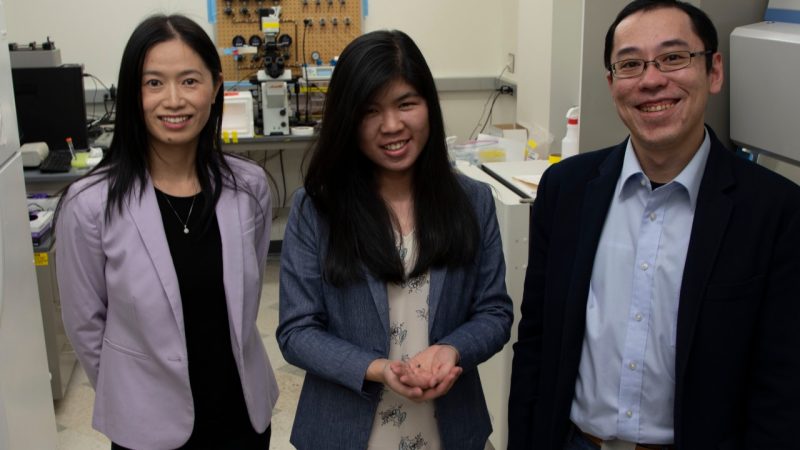
Tong came to Virginia Tech in 2015, the same year that Assistant Professor Xiaoting Jia joined the Bradley Department of Electrical and Computer Engineering. When the two met, they began discussing their respective research — his experience in drug delivery and cancer immunotherapy and hers on optical fibers for sensing neurological diseases.
Deciding to merge their efforts to help combat cancer, Tong and Jia addressed the problem with current immunotherapy delivery methods by working on a project to develop a miniature optical fiber treatment device that can deliver cancer immunotherapeutic antibodies while measuring tumor impedance to monitor treatment efficacy.
Their initial team included their first graduate students, Ai Lin Chin, a Ph.D. student in chemical engineering (projected to graduate this fall) and Jiang Shan, who received a Ph.D. in electrical engineering in May 2021 and is currently a post doc researcher at Stanford University. Subsequently, Eungyo Jang and Liqian Niu, Ph.D. students in chemical engineering advised by Tong; and Liwu Li, professor of biological sciences, an expert in immunology, joined the researchers.
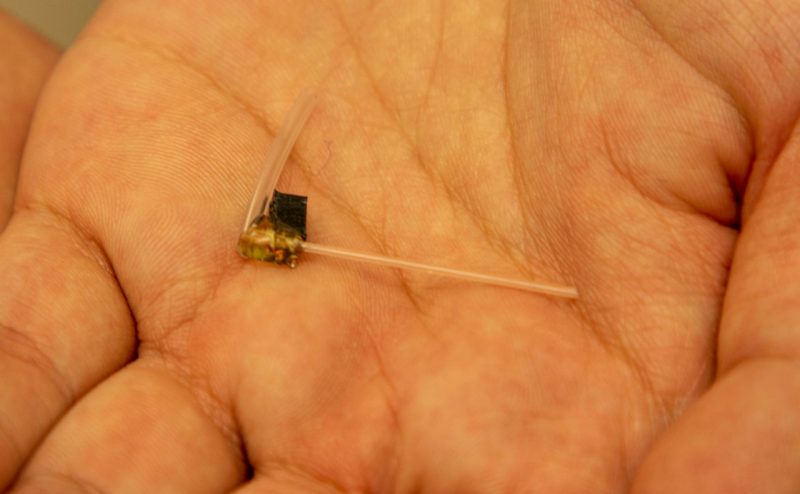
By using electrode-embedded optical fibers, which have both local delivery and measurement capabilities that span the course of a few weeks, and combining local immune checkpoint blockade antibodies delivery with photodynamic therapy, the researchers have been able to elicit a sustained anti-tumor immunity with complete tumor shrinkage in multiple tumor models. To test whether the cured mice have “immune memory” against tumors, the researchers challenged the cured mice by injecting tumor cells into these mice, and they found that none of the cured mice had tumor re-growth.
“We can infuse antibodies through our miniature fiber to the tumor to activate T cells around tumor cells and further elicit anti-tumor immunity by recruiting more T cells to the tumor bed,” said Jia. “This will eventually produce strong and durable anti-tumor immunity as we see the accumulated memory T cells in tumors and lymph nodes.”
The team’s delivery approach, from local to systemic, is very different from conventional treatment that uses only a systemic administration method, said Tong. And it also avoids antibodies causing toxicities before reaching the tumor.
Tong said the research found that measuring tumor electrical signals (tumor impedance) using the new device is rapid and allows real-time monitoring of tumor growth, which differs greatly from conventional contrast-agent based tumor imaging therapies.
“When a tumor grows up, the impedance reading correspondingly increases; when tumor sizes decrease because of the antibodies treatment, we also find the impedance decreased,” Jia said.
A paper explaining their work, “Implantable optical fibers for immunotherapeutics delivery and tumor impedance measurement,” was recently published in Nature Communications, an open access, multidisciplinary journal dedicated to publishing high-quality research in all areas of the biological, health, physical, chemical and Earth sciences. Papers published by the journal aim to represent important advances of significance to specialists within each field.
“Jia and I began this research as young, enthusiastic faculty members at Virginia Tech who were hopeful but not really sure of the result,” said Tong. “We are very pleased with the contribution our collaboration has made to achieving better results for patients undergoing cancer immunotherapy and we encourage other young professors in the College of Engineering to join forces that could open up new possibilities in the biomedical engineering field.”





