Providing health care in the digital age
Transdisciplinary research team members

Health equity and access, especially in rural, underserved communities, is a complex problem, and complex problems require innovative solutions. That’s why one transdisciplinary research team is working across traditional academic barriers to increase health care access to vulnerable populations.
The integrated Translational Health Research Institute of Virginia (iTHRIV) has selected Elham Morshedzadeh and Melinda Schriver as the principal investigators working to create an interactive training system for telemedicine cart users to increase health care access across Virginia. Morshedzadeh currently serves as assistant professor of industrial design in the School of Architecture and Design, while Schriver serves as the director of Digital Health at Carilion Clinic. iTHRIV is a collaborative program funded by the National Center for Advancing Translational Sciences of the National Institutes of Health (NIH).
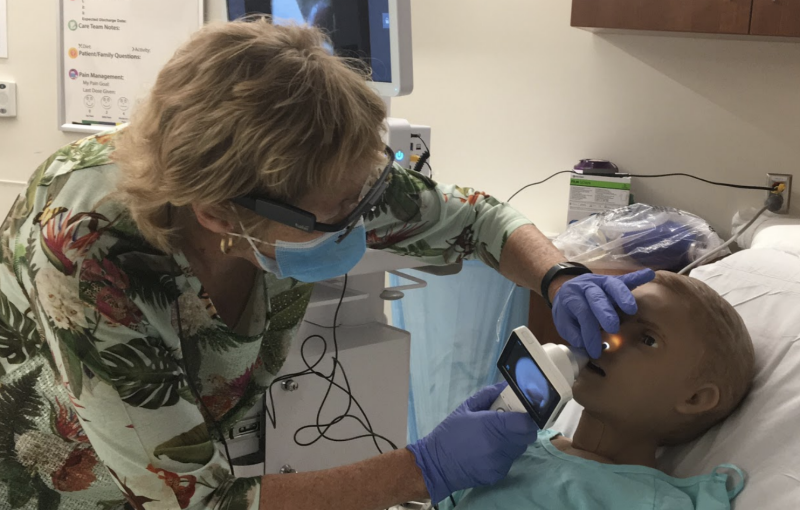
Telemedicine is a broad term that refers to health care from a distance. Ranging from a simple phone call to video conferencing, telemedicine allows physicians and specialists to interact with patients from across the state, country, or world. As Morshedzadeh explains, in addition to audio-visual technology, “telemedicine carts have peripheral devices and attachments that can collect vital data of patients like heartbeat and breathing quality. They can look into the ear and eyes, the same way that a doctor or a nurse practitioner would in a routine exam.”
Telemedicine cart training
If there’s a silver lining to the ongoing pandemic, it’s that the need to interact from afar has given rise to innovative technology.
“COVID-19 has broken a lot of the barriers,” explained Andre Muelenaer, a team member and professor of practice in biomedical engineering. During his 40 years of clinical work, the Virginia Tech alumnus witnessed the evolution of telemedicine at Carilion, from the early days of over-the-phone telepsychiatry to the multifaceted and interactive full examinations made possible by telemedicine carts.
But while the technology is becoming more accessible, practitioners learning and becoming comfortable with the technology is still a barrier to underserved areas.
“The equipment and devices are being designed and made available, but with a lack of proper training, they are not being used to their full potential,” Muelenaer said.
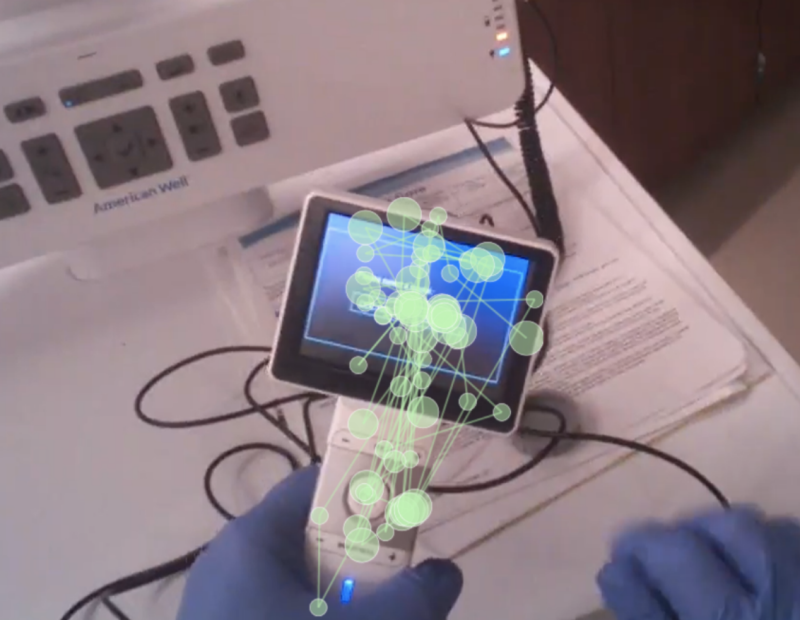
That’s where the research team is concentrating its efforts. Focusing on pediatric nurses and medical practitioners, the first phase of the project began last summer by identifying “pain points” for users — the specific areas of concern with using the carts. Pain points for nurses included specific problems with the cart design and communication concerns. This issue identification led to plans for designing an initial training system integrating experiential learning and augmented reality, for which the team hopes to involve live patients in the next phase.
Wallace Lages, an assistant professor of creative technologies in the School of Visual Arts, will be contributing his expert knowledge in augmented and virtual reality technology.
“We are hoping that practitioners can become familiar enough to perform the exam session,” Morshedzadeh said of the project goal.
Eye tracking data
Training cart users isn’t the only educational benefit of this initiative. Phase One of the study included assistance from students Michelle Morris, a junior majoring in biomedical engineering and mechanics, and seniors Dana Werlich and Olivia Menezes, majoring in industrial design. The trio was selected after participating in Morshedzadeh’s undergraduate course on needs identification in health care. In addition to hands-on experience, they all realized the benefit transdisciplinary research has for both scholars and target populations.
Menezes expressed her appreciation for the opportunities afforded her and her colleagues.
“Having access to that kind of technology is a real privilege," Menezes said. "Using tools to collect information that can inform how people interact with things — I think that that's pretty huge.”
Morris, who comes from rural Abingdon, Virginia, also spoke of the benefit to communities.
“Telemedicine is definitely beneficial for people in rural areas, especially children who would otherwise have to take an entire day off of school to go to a specialist," Morris said. "With telemedicine, they could just miss a single class if they were able to go to their local provider.”
Echoing Morris' comments, Werlich concluded, “for those that do not regularly have access to health care, this is something that could give them the access if they have the correct tools and the correct system in place.”
Ultimately, the project is about establishing trust among researchers across fields, the users of technology, and the populations in need.
“We are working to create an experience that builds trust," Morshedzadeh said. "When community members trust this technology, they will share their experience with other community members. This acceptance is crucial to building greater health care access.”
- Written by Phil Miskovic




