Transformative alliance: Health leaders, Virginia Tech forge new partnership for diabetes management and support

Virginia Tech Cooperative Extension has partnered with the National Association of Chronic Disease Directors (NACDD) to explore how a diabetes social support program developed by Centers of Disease Control (CDC) can help people manage their diabetes.
Over 630,000 people in Virginia have diabetes. Not only is diabetes associated with an increased risk of diseases like heart disease and stroke, but if left untreated, serious complications such as kidney damage and vision loss can arise, which makes diabetes management an urgent topic.
"Cooperative Extension is very focused on how to serve communities depending on what they say their needs are. Each of our 107 units use publicly available data in addition to surveys and interviews in their communities to find out what their perceived needs are — and they're concerned about diabetes,” said Kathy Hosig. Hosig serves as the director of the Center for Public Health Practice and Research at the Virginia-Maryland College of Veterinary Medicine, and she is a public health specialist with Virginia Cooperative Extension.
CDC’s program “New Beginnings: A Discussion Guide for Living Well with Diabetes” focuses on discussion and community-building to improve health and quality of life for people with diabetes. It’s been used by support groups and diabetes education specialists for decades, but its efficacy has never been formally studied — this is where NACDD and Virginia Cooperative Extension come in.
When most people hear Cooperative Extension, their mind jumps to agriculture and 4-H programs, but Extension offers so much more: working through land grant universities, Extension brings a wide range of educational opportunities into communities through local Extension offices.
"In many states, the fastest-growing part of Extension is Health Extension, integrating Extension's rural footprint, educational efforts, health, nutrition, as well as community and its connection to the food system to really start addressing public health issues,” said Mike Gutter, director of Virginia Cooperative Extension and associate dean of the College of Agriculture and Life Sciences.
"There's a growing acknowledgement that public health and Extension are really one in the same: what we do with Extension is really public health,” said Hosig.
In her role as Extension public health specialist, Hosig developed a program called Balanced Living with Diabetes (BLD) that educates people with type 2 diabetes on topics like exercise, carbohydrate intake, and the importance of taking medication to manage their diabetes. BLD has been used successfully in Virginia communities for over a decade.
CDC awarded a grant for Virginia Cooperative Extension and NACDD to work together to use the BLD program’s infrastructure to study how New Beginnings affects diabetes management through enhancing social support.
They can do this thanks to one of Extension’s greatest strengths: connection to community.
Extension agents have long been embedded in local communities and have established relationships with community leaders, granting them the trust and confidence they need to carry out educational programs.
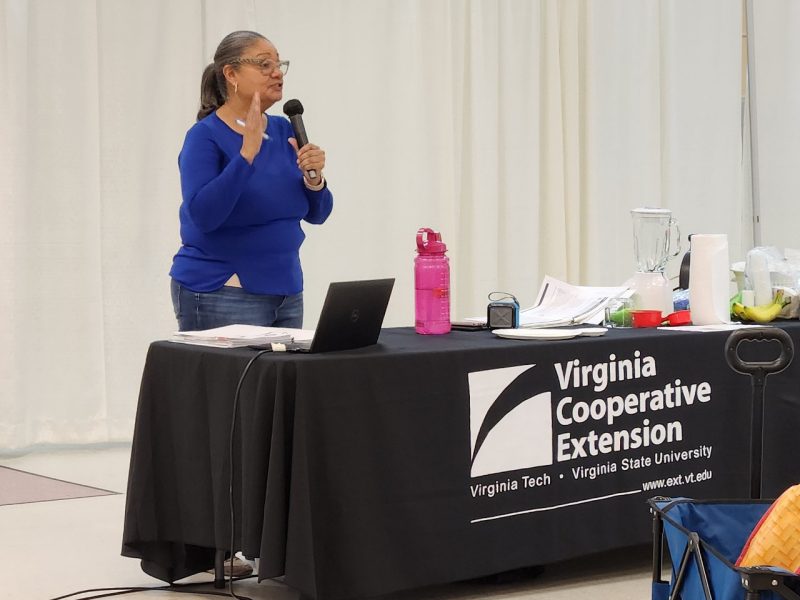

BLD is geared towards people with type 2 diabetes who don’t want to go to a clinical location for their diabetes education. Many people face financial barriers or lack transportation access, keeping them from going to the doctor’s office, but Extension brings the education to them, working at places like faith-based organizations, YMCAs, and senior centers. Extension partners with local certified diabetes care and education specialists or registered dietitians who teach at least two of the program sessions, emphasizing physiological and clinical aspects of diabetes. Extension agents coordinate and lead the program. They teach the remaining sessions and demonstrate exercises and preparation of recipes that meet recommendations for people living with type 2 diabetes.
The BLD program runs for six weeks, takes an eight week break, then resumes for a final meeting. In the first meeting and the reunion meeting, participants’ blood sugar is measured through the A1c test, which measures the average blood sugar level over the past three months.
Over the next year and a half, however, participants at each location will be split up into two groups. One group will go through BLD like normal. The other group will do the first six weeks of BLD, but instead of taking an eight week break, they will go through the New Beginnings curriculum. The first class, hosted by a large church in Richmond, has already begun!
In addition to measuring participants’ A1c level, the research team will distribute questionnaires to gather more information, and public health students at the college will be invited to get hands-on experience collecting and inputting data. Kristina Jiles, public health Extension specialist and research assistant professor in the Center for Public Health Practice and Research, will develop a training module to help Extension agents run New Beginnings, adding consistency to how the program is led.
People with diabetes can get advice from their doctors, so why are programs like BLD and New Beginnings important?
Researchers have found that the social element plays a key role to getting care — once people establish a relationship with a diabetes educator, they’re often more motivated to actually set up an appointment with their doctor. After all, going to the doctor can be intimidating. Some also follow up with a hospital-based diabetes education program for more intensive individual diabetes self-management education.
"A lot of it is the fear of the clinical setting and the way we approach carbohydrate control. When you go to a clinical setting, people are often told to keep track of grams of carbohydrates,” Hosig said.
On the other hand, she explained, people in BLD are taught the plate method: on a 9-inch plate, foods with carbohydrates should take up no more than a quarter of the plate. By emphasizing proportions over numbers, BLD participants are taught a more practical method of managing their carbohydrate intakes. The program also shows them how to perform low-intensity exercises, and participants practice the exercises together so they can feel confident doing them at home.
Programs like New Beginnings give people the social support and encouragement they need to develop sustainable, healthy skills and habits.
"We expect A1c levels to be lower in the group that got the social support — they have more support from their family, from their care providers, and other people in their communities to control their carbohydrate intake and go for walks. We also expect that having that Extension agent with them for an additional seven weeks and bringing in community resources, that they will have better outcomes," said Hosig.
Through this partnership, Extension will gather information that will help even more people with diabetes lead healthier lives.
"Diabetes prevention and management programs are an absolute great fit for Cooperative Extension, and in Virginia, they've had profound success,” said Gutter.
"Extension is honored to be partnering with these groups and doing what we can do to address a big challenge for many Virginia families. We're glad to be part of this solution at work.”
Team members involved in the project:
- Kristina Jiles (PHS and Extension/CALS): Co-investigator and Extension lead for Balanced Living with Diabetes program
- Lisa Homa (PHS): Project Coordinator and Evaluator
- Elizabeth Caton (PHS): Research team member
- Alex Hanlon, Alicia Lozano and Rachel Silverman (Statistics/COS): Biostatisticians




