Detecting COVID-19 in the air
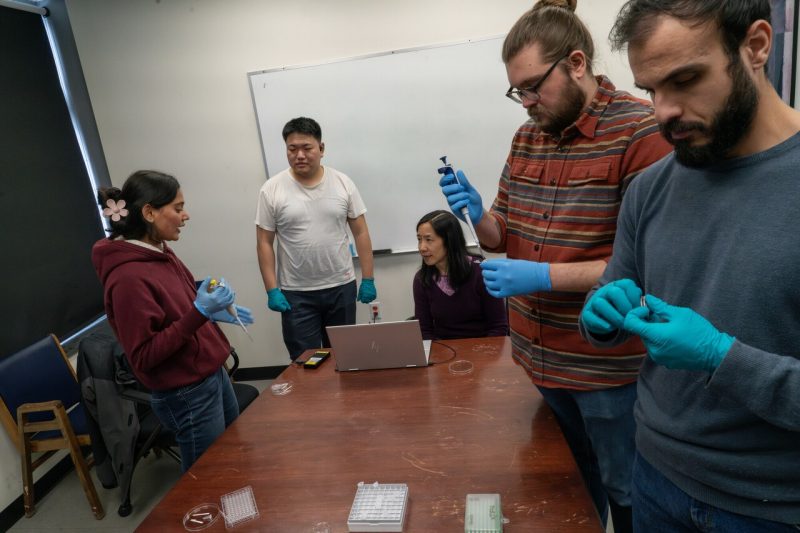
A team of more than a dozen faculty, postdoctoral researchers, and student researchers are combining their expertise to develop a device that can assess the environmental risk of COVID-19 transmission in real time.
A popular piece of outdoor equipment and a medical industry staple are helping Virginia Tech researchers move closer toward a low-tech detection tool for airborne illnesses.
“The main issue we were having was how can we collect enough air as fast as possible and in a relatively cheap way,” said Christos Stamatis, a postdoctoral researcher. “The best material we found was the combination of the surgical mask and the dry bag.”
Stamatis is one of more than a dozen faculty, postdocs, and student researchers who are combining their expertise to develop a device that can assess the environmental risk of COVID-19 transmission in real time. Led by University Distinguished Professor Linsey Marr, the team has made great strides in figuring out how to successfully capture the necessary amount of air, filter it, deposit it onto a test strip, and identify virus particles.
“Determining the amount of virus in the air is really important to avoid getting sick,” said Marr, the Charles P. Lunsford Professor of Civil and Environmental Engineering. “We have wastewater data that tells you what’s been going on in the community a day or two after testing, but you want to know what’s in this room with the air I’m breathing now.”
The exploratory project was funded by Wellcome Leap, a nonprofit organization working to accelerate innovations that transform human health.
“The challenge was, if an individual walks into a movie theater, an airplane, a shopping mall, how can they know if there’s enough virus in the air that they should be worried about entering or about having a gathering in that room,” Marr said. “Currently, there are ways to collect an air sample from a room, but they involve big, noisy pumps, and it’s a few days later when you find out how much virus was in the air. So the challenge here was to help the individual who doesn’t have access to that and who needs to know within about 15 minutes. And if we can do that, people can make better decisions that ultimately will benefit the health of entire communities.”
More specifically, the research team had three primary objectives:
- Collect a large enough air sample without using electricity
- Get the sample into liquid – concentrating or enriching the virus to stand out against a background of lots of dust
- Utilize antibodies and Raman spectroscopy – an approach commonly used in chemistry to provide a structure fingerprint for molecules so they can be more easily identified - to detect the virus
Marr said the first step proved to be the most daunting part because unlike a liquid, which can easily be easily obtained in something like a cup, there wasn’t a ready-made device for capturing a large amount of air and shrinking it into a droplet.
Stamatis was among those tasked with experimenting with this particular aspect of the project. He said after trying a variety of devices, including fans from computer processors, the team landed on using a dry bag - a waterproof bag commonly used during outdoor activities – to capture the air.
“We didn’t want it to be so hard people were sweating trying to do it, but we also needed to get a large enough air sample,” Stamatis said.
Once trapped, the air is squeezed toward a 3D-printed filter holder attached to the bottom of the bag and containing a filter cut out of a standard surgical mask. The filter is then removed and placed in a liquid that contains antibodies and nanoparticles, and the liquid is then dropped onto a test strip, which is analyzed by the Raman spectroscopy.
The project is likely a year or two away from being developed for public use, but the team’s progress is a substantial step toward that end goal. And once successful, could likely be a platform for detecting a range of other airborne illnesses.
“A lot of other people are working on these types of devices, but I think what sets us apart is that we are thinking about detecting the virus at very low, realistic levels in a background of tons of other types of particles in the air and doing so in a way that doesn’t require heavy, power-hungry sampling pumps that can be hard to use in an occupied space,” Marr said.
Virginia Tech is one of 21 charter members of the Leap Health Breakthrough Network, which along with the nonprofit, was founded by the Wellcome Trust.
Along with Marr as the principal investigator, the research team has four co-principal investigators:
- Peter Vikesland, the Nick Prillaman Professor of Civil and Environmental Engineering
- Wei Zhou, associate professor of electrical and computer engineering
- Nisha Duggal, associate professor of virology
- Gabriel Isaacman-VanWertz, associate professor of civil and environmental engineering
Sonali Srivastava, a graduate research associate on the project, said the project’s interdisciplinary nature was a great benefit to her educational journey.
“I did not have any idea about the biology aspect of this work, for example,” said Srivastava, who is studying civil and environmental engineering. “But working with a range of people from the biology department to electrical engineering, I learned a lot from each one of them.”
Similarly, Stamatis said the project’s interdisciplinary nature was what drew him to it in the first place.
“The reason I asked to be a part of the project is the fact that is was going to be so multidisciplinary,” Stamatis said. “You usually don’t get the chance to work that often with other fields, and out in the world, when you design a project, you have to work with people from different fields.”




