Cancer researchers team up against deadliest brain tumors in children
Experts from Children's National, Virginia Tech, and Columbia University join forces to explore new tactics to fight lethal childhood brain cancer.
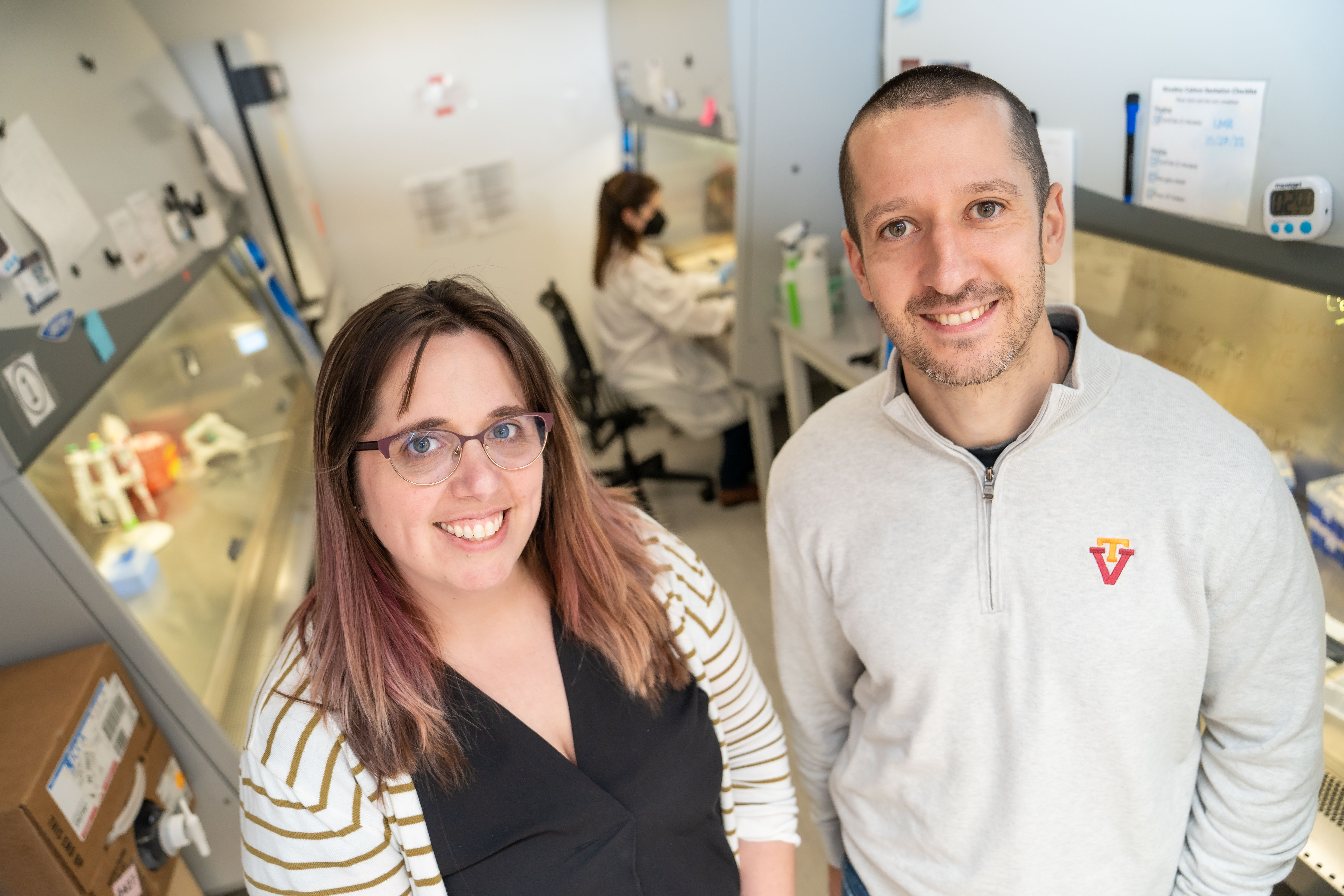
Jennifer Munson and Javad Nazarian of Children's National Hospital Javad Nazarian, a principal investigator with Children’s National Hospital, will study how to use focused ultrasound to create a temporary gateway through the body’s protective blood-brain barrier to deliver cancer medicine.

Virginia Tech researchers with the Fralin Biomedical Research Institute at VTC have joined a Children’s National Hospital effort to treat deadly brain tumors with ultrahigh frequency sound waves.
The scientists are studying how to use an emerging technology called focused ultrasound to fight diffuse midline glioma (DMG), one of the most lethal childhood brain cancers with a nearly 100 percent rate of mortality within five years of diagnosis.
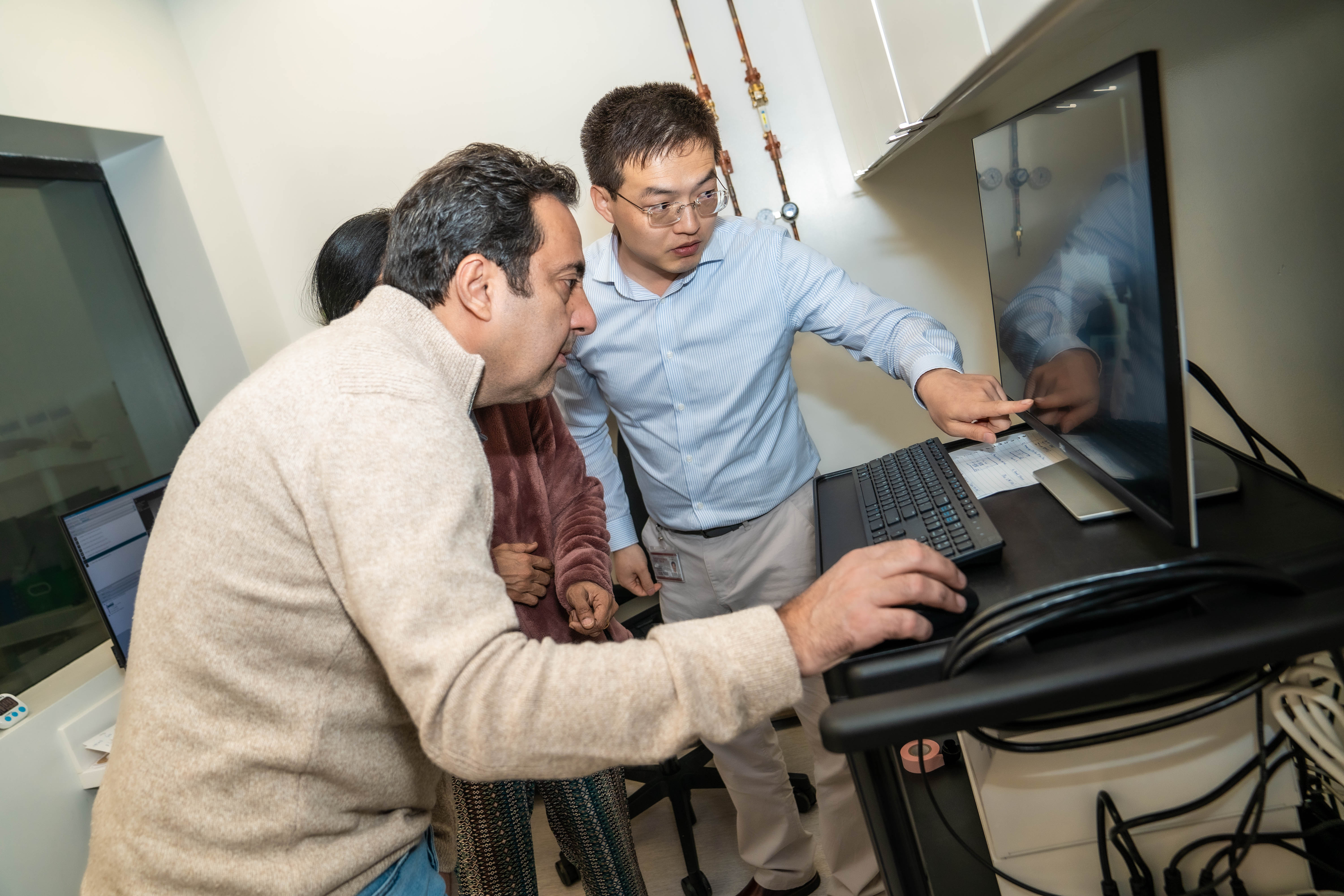
A multi-institutional team led by Javad Nazarian, a principal investigator with Children’s National Hospital, will study how to use focused ultrasound to create a temporary gateway through the body’s protective blood-brain barrier to deliver cancer medicine.
Virginia Tech Cancer Research Alliance investigators Eli Vlaisavljevich, a designer and developer of focused ultrasound technology, and Jennifer Munson, who creates 3D models to study brain tumors, bring expertise in focused ultrasound instrumentation and tissue engineering to the team.
Joining them is Columbia University’s Cheng-Chia Wu, principal investigator for the world’s first clinical trial using focused ultrasound in children with relapsed DMG. Wu is experienced in combining focused ultrasound with radiation and immunotherapy for both pediatric and adult brain tumors.
“Bringing this expertise together will advance this promising platform for treatment of pediatric brain tumors,” Nazarian said. “Individually, we progress slowly or we may fail. Together, we will be able to better understand how to treat these tumors and accelerate their delivery to the clinic.”
The research is funded by a $672,000 grant to Children’s National from the SebastianStrong Foundation, a nonprofit organization that raises awareness of childhood cancers and provides support for less toxic, more targeted childhood cancer treatments and cures.
At Virginia Tech, the project springs from research supported by an earlier Seale Innovation Fund grant issued through the Fralin Biomedical Research Institute to Munson, Vlaisavljevich, and Nazarian. That study centered on focused ultrasound and sonodynamic therapy, which is a noninvasive tumor treatment that reduces the number of cancer cells and discourages future tumor growth.
“You can't hit these deadly, invasive tumors in children with the aggressive treatment we do in adults because it can cause damage and harm a child’s development,” said Munson, associate professor of the Fralin Biomedical Research Institute and the Department of Biomedical Engineering and Mechanics in the College of Engineering. “We want to reach these tumors with effective treatment doses, but without causing damage.”
Munson's lab will develop 3D cell culture models that include DMG tumor cells from Children’s National patients. The 3D tissue-engineered model of the tumor microenvironment can reveal why the tumors return and which treatments will be most effective at eradicating them.
“Our goal is ultimately to develop a personalized medicine approach in which we can take a patient's tumor, build a model of that tumor in a dish, test drugs on it, and tell a clinician which therapy will work best to treat it,” Munson said.
Meanwhile, Vlaisavljevich will design focused ultrasound instrumentation to work in cell cultures as well as living systems. Vlaisavljevich’s Therapeutic Ultrasound and Noninvasive Therapies lab at Virginia Tech explores a technology called histotripsy, which is used to generate cavitation bubbles in tissue that, when popped, have the ability to destroy targeted tumors.
“The problem is delivery — actually getting the drug to the target. That's difficult in the brain,” said Vlaisavljevich, associate professor in the Department of Biomedical Engineering and Mechanics. “One of the promising benefits we’ve seen is focused ultrasound can be used in combination with microbubbles to open the blood brain barrier and allow drug delivery into tumors that are normally hard to reach for any type of therapeutic approach.”
DMG tumors often begin in the base of the brain near the spinal cord and travel through the central nervous system via cerebrospinal fluid, which makes surgery, radiation, and chemotherapy difficult. What’s more, the tumor can invade nearby tissue and extend beyond what can be seen on MRI or by the surgeon during surgery, according to the National Cancer Institute.
“Our portion of the project is to conduct fundamental science,” Vlaisavljevich said. “We can look at how to tailor this therapy to have the most effectiveness against cancer cells, with minimal off-target effects and reduced toxicity.”
Research to find solutions for pediatric cancer is desperately needed, according to Oscar Ortiz, who founded the SebastianStrong Foundation in 2017 in memory of his son Sebastian, who died of cancer.
“Only a handful of drugs have been specifically created for fighting childhood cancer since 1980, while in that same time period hundreds have been made for fighting cancer in adults,” Ortiz said. “Kids deserve so much better.”
The study will take place at Virginia Tech labs on the Blacksburg campus and at the Fralin Biomedical Research Institute in Roanoke, with ongoing research for the project under way at the Children’s National Research & Innovation Campus in Washington, D.C.
Meanwhile, in complementary efforts, Kathleen Mulvaney and Jia-Ray Yu, assistant professors with the Fralin Biomedical Research Institute whose research programs are housed at the Children’s National Research & Innovation Campus, are pursuing research strategies for identifying new leading edge approaches to identifying and delivering new therapeutic interventions at a molecular level to treat childhood brain cancers.
Yu explores the epigenetic and molecular foundation of diffuse midline glioma to find potentially new therapies, while Mulvaney seeks to exploit weaknesses in two rare but lethal cancers that affect children: glioblastoma and malignant peripheral nerve sheath tumor. Their goal is to develop together and in parallel therapeutic approaches that can treat a range of pediatric brain cancers.
May is Brain Tumor Awareness Month and National Cancer Research Month.





.jpg)
