Virginia Tech researcher’s 3D model of brain tumor environment could aid personalized treatment
Jennifer Munson and her research team’s model of the glioblastoma tumor microenvironment could help with understanding why the cancer is so resistant to treatment and so often returns after surgery.

Glioblastoma, a rare but deadly brain cancer, is wickedly sturdy. Surgeons remove tumors only to see the cancer come back ferociously. Chemotherapy and radiation therapy have limited effects. About half of patients die within 18 months.
But now Virginia Tech scientists have developed a novel 3D tissue-engineered model of the glioblastoma tumor microenvironment that can be used to learn why the tumors return and what treatments will be most effective at eradicating them – right down to a patient-specific level.
The model and its development are described in a paper published July 29 in Nature Partner Journals Precision Oncology.
“Our goal is ultimately to develop a personalized medicine approach in which we can take a patient's tumor, build a model of that tumor in a dish, test drugs on it, and tell a clinician which therapy will work best to treat it,” said Jennifer Munson, associate professor at the Fralin Biomedical Research Institute at VTC and the paper’s corresponding author.
The model is an important step to identify new markers and therapies for the cancer. Research using the new model has already identified a new measure for understanding a patient’s tumor, including the capability of the cancer cells to renew and differentiate themselves, which is an indicator of how the cancer will respond to drug treatments.
About 15,000 people a year are diagnosed with glioblastoma, according to the National Cancer Institute.
Munson, a tissue engineer who is also an associate professor in Virginia Tech’s Department of Biomedical Engineering and Mechanics and one of the co-directors of the Virginia Tech Cancer Research Alliance, began developing the models in 2014. While other engineered models exist, this one accounts for cell types other than tumor cells, along with the space for the tumor to grow and spread, and other aspects of the actual tumor microenvironment.
Munson’s models, which are typically about the size of a pencil eraser, more accurately recreate that environment for study, including cells unique to the central nervous system such as astrocytes and microglia, and in ratios based on those found in patients.
The model also considers the movement of fluid between and around cells in tissues — known as interstitial fluid flow — which is known to increase in tumors and speed the cancer’s spread. Fluid flow in the model also allows for easy testing of drug therapies.
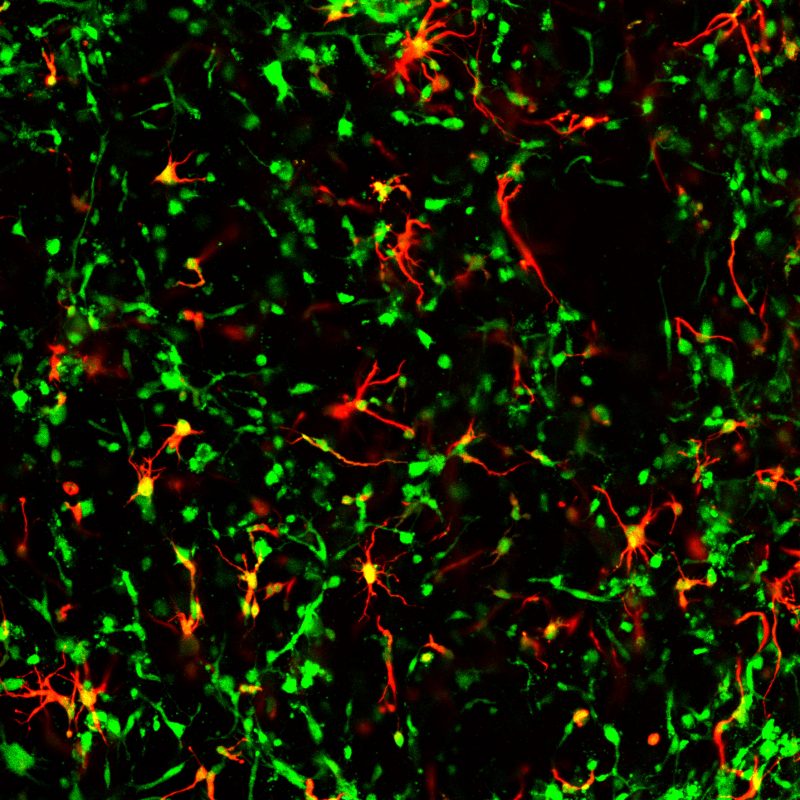
The microenvironment is crucial to understanding why glioblastoma is so difficult to treat. Though a tumor can be removed, tumor cells tend to invade the surrounding tissue where they become more harmful or resistant to therapies, allowing the cancer to return.
“We wanted to mimic that environment as closely as possible because that is what you would be later treating with drugs or doing any sort of follow up treatment,” Munson said.
Munson and her team have used the models to test the impact of different treatments, analyzing for how cancer cells invade tissue, how they proliferate, their ability to renew themselves, and how many cells die. They found results varied widely, which highlights the importance of a personalized medicine approach to glioblastoma and the value of being able to recreate an individual patient’s tumor microenvironment.
“The model can help us answer questions like, can we predict therapeutic response?” Munson said. “Can we see how these different cell types contribute to tumor cell behavior, or can we just better understand this microenvironment that allows physicians to more effectively treat patients who typically have a poor chance of survival?”





