Scholar award helps doctoral student advance cancer treatment while enhancing representation

With a background in radiation therapy and current research focused on novel cancer therapies, Sabrina Campelo has a unique perspective on the application of physics in the world of cancer care. Campelo, a doctoral student in the Virginia Tech-Wake Forest University School of Biomedical Engineering and Sciences program, will continue her innovative work in translational cancer research with the help of the nonprofit Philanthropic Educational Organization (P.E.O.) Scholar Award for the 2022-23 academic year.
“Almost everyone knows someone affected by cancer,” said Campelo. “For me, a lot of family members have passed from cancer. As I saw more and more people dying or suffering from side effects of treatment, I knew I wanted to do something to help. It just seemed unacceptable to me.”
In high school, a great-aunt living with Campelo was diagnosed with and lost a battle to cancer. Soon after, a classmate’s 11-year-old sibling was diagnosed with glioblastoma, a devastating brain tumor. Campelo followed the child’s journey, from diagnosis to chemotherapy, and watched as the tough side effects culminated in another heartbreaking experience. Some of the radiology treatment side effects included severe exhaustion, dry and itchy skin, and hair loss.
“It was horrible seeing them suffer from the side effects of their treatments,” she said.
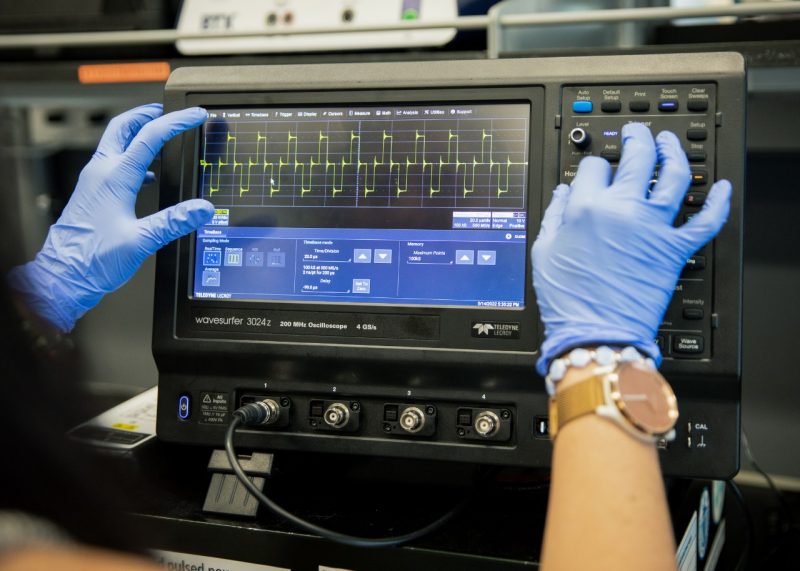
Bearing witness to the cruelty of cancer led her to the academic fields of physics and engineering with the hope of finding less harsh treatments for patients with tumors. With a background in radiation therapy, Campelo chose Virginia Tech so she could study translational cancer research in the Bioelectromechanical Systems Laboratory. Under the guidance of Rafael Davalos, the L. Preston Wade Professor in biomedical engineering and mechanics in the College of Engineering, the lab’s researchers are making strides with high-frequency irreversible electroporation, a novel cancer therapy.

The technique uses minimally invasive probes to deliver low-energy pulses to targeted tissue, a process that kills diseased cells by destabilizing their membranes. This method uses electric fields around the targeted cells and delivers pulses that ablate – or induce cell death – in the cells closest to the pulse and temporarily disrupt more-distant surrounding tissue.
Notably, the minimally invasive procedure targets cancerous cells rather than healthy ones. Furthermore, its precision enables treatment near critical structures such as major blood vessels and nerves, allowing clinicians to target previously unreachable tissue. This technology received the Expedited Pathway Designation from the U.S. Food and Drug Administration in 2018 and has been used to help thousands of patients worldwide.
Campelo’s current research on high-frequency irreversible electroporation is twofold. First, the therapy has proven highly effective in targeting and killing cancerous cells. As a method of cancer treatment, it has more than doubled the median survival time of stage III pancreatic cancer patients. It also has been used to successfully treat patients with prostate, liver, and kidney cancers.
Beyond that, Campelo wants to learn more about the method’s use of pulses that can disrupt the blood-brain barrier.
“The blood-brain barrier is important and helpful to protect the nervous system from circulating toxins,” said Campelo. “When we need a drug to break through the barrier, however, that’s when the barrier is problematic. Some brain cancer drugs may not be able to penetrate the blood-brain barrier, so I am fine-tuning the use of pulses to temporarily disrupt the barrier for drug delivery to the brain.”
This innovation could transform standard-of-care cancer treatment, resulting in fewer side effects while still targeting — and destroying — cancer cells. Campelo wants to cultivate this new technology and raise awareness for clinical use.
“I am motivated to be a leader in the field,” said Campelo. “I also want to bring representation of minorities. Having P.E.O. supporting me as a woman means a lot, and I want to pay that forward. It’s important to bring visibility to women in these fields and to show others, ‘Yes, you can.’ You, too, can be successful in these fields.”
According to the Pew Research Center, more women than men have graduated with their bachelor’s degrees in recent years. This trend of women advancing their education has been steadily increasing since the 1970s.
With a mission to help women advance in education, P.E.O. has awarded nearly $400 million in grants, scholarships, awards, and loans. Since its inception in 1869, P.E.O. has helped more than 119,000 women pursue educational goals.
Campelo said she is grateful to have the benefit of joining a diverse lab – including an atmosphere of respect and support – with a good balance of men and women, as well as having other Hispanic colleagues, including the director, Davalos.
“As the child of a Colombian immigrant and a Cuban refugee, I was raised on the basis that almost anything could be accomplished if the effort, passion, and persistence were there,” said Campelo. “My parents emphasized the power of education and helping those who are in need. With this degree, I hope to help others through cancer treatment options.”
Campelo received her bachelor’s degree in physics with minors in biology and applied mathematics from Elon University. She received her master’s degree in medical physics from Duke University. She plans to return to medical physics as a clinical professional after graduating with her Ph.D. from the School of Biomedical Engineering and Sciences.
Related Stories
- Rafael Davalos named American Institute for Medical and Biological Engineering Fellow
- A dog lives on; now the stage is being set for treating humans
- Shocking the cellular world: Engineers’ collaborative work discovers force signature of cells undergoing electroporation
- Ph.D. students bring research-backed insights on inclusive action to film series on women in science




