Scientists identify neural disruptions underlying feeding, swallowing disorders in children
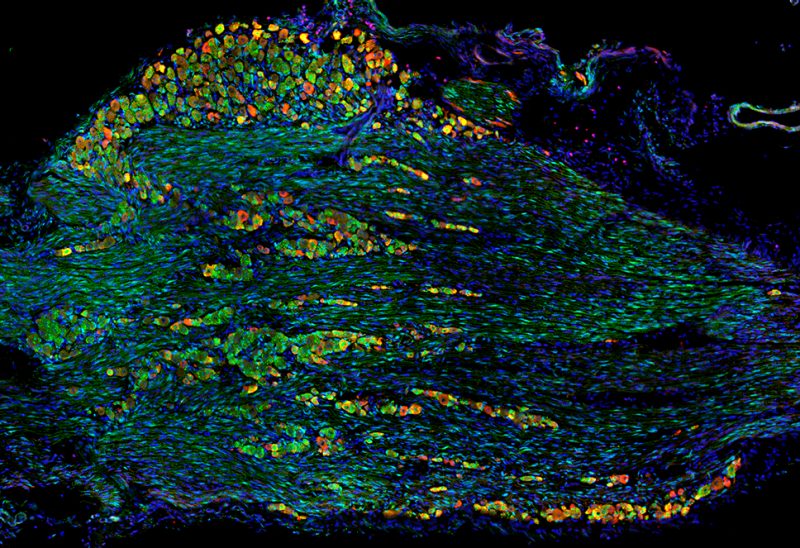
Neuroscience team led by Professor Anthony-Samuel LaMantia of the Fralin Biomedical Research Institute at VTC shed insight on early cellular interactions underlying cranial nerve development.
Every time you chew food, talk, yawn, or sense the zap of a toothache, cranial nerve cells are shuttling electrochemical signals to your brain. Some of these neurons detect pain, while others sense facial muscle movements or sensations in the skin.
Now, in a new study published in Disease Models & Mechanisms, Fralin Biomedical Research Institute at VTC scientists led by Anthony-Samuel LaMantia depict the early development of pain-sensing and movement-sensing neurons in the face and throat. The findings reveal a previously unexplored feature of brain and cranial nerve development underlying eating, swallowing, and speech.
“We were able to show for the first time that this momentary interaction between two groups of cells plays a crucial role in regulating movement and pain-sensing innervation in the face,” LaMantia, professor and director of the Fralin Biomedical Research Institute’s Center for Neurobiology Research.
The researchers examined early neural development in mice embryos with DiGeorge syndrome, a rare genetic disorder associated with neural and facial abnormalities. Like human patients born with DiGeorge, mice can carry the identical genetic mutation, providing an ideal model to study where development goes awry at the cellular and molecular level.
Children born with DiGeorge commonly have trouble coordinating suckling and swallowing milk, a condition called pediatric dysphagia, but it’s unclear how the mutation causes these functional abnormalities. While mouth, tongue, and throat movements involved in eating are controlled by motor neurons, mechanosensory neurons – a subject of this study – detect and integrate movement signals to fine-tune the behavior. The study also evaluated pain-sensing neurons, or nociceptors, which monitor potentially harmful aspects of eating behavior, including excessive temperatures and irritants like capsaicin in hot peppers.
LaMantia and his laboratory have been studying this syndrome to disentangle facets of cranial nerve development and oropharyngeal behaviors for a decade.
Based on their prior research, the scientists knew that on day nine of mouse embryo development, two groups of cells – neural crest and placode cells – needed to meet to begin blueprinting the facial nerve. They knew that in the syndromic mice, something went wrong at this stage of development that had deleterious behavioral consequences, but it needed further investigation.
“Starting out, we weren’t sure if these two groups of cells just weren’t migrating together to meet in the proper place, or if they were in the right place at the right time, and just failed to communicate,” LaMantia said.
With this newly published data, LaMantia’s lab now suspects the latter is true.
Combining in vivo analysis and imaging to visualize a variety of molecular markers, the researchers found that neural crest cells were turning into pain-sensing neurons far too soon. This premature differentiation caused the quantity of placode cells, which become mechanosensory neurons, to increase relative to neural crest cells.
This study builds on previous work by LaMantia’s lab. Seven years ago, the researchers examined if the developing cranial nerve neurons were growing axons that met functional targets in the face, mouth, and throat. They found that compared with ordinary mice, the syndromic mice embryos lacked proper innervation – the axons were shorter, misplaced, and disorganized.
“Not only were the neurons confused about what they were supposed to do, their axons also didn’t have precise destinations – they just got lost,” LaMantia said.
In a follow-up study, LaMantia’s lab identified key genes involved in regulating normal axonal growth in the cranial nerve. Remarkably, the researchers were able to restore ordinary cranial nerve growth in mice with DiGeorge syndrome by suppressing a specific gene.
The new discovery reveals how changes in gene expression associated with DiGeorge syndrome destabilize sensory neuron growth by interrupting a key interaction between neural crest and placode cells. LaMantia’s lab now aims to uncover the molecular signals that these cell groups need to assemble a healthy cranial nerve.
“Now that we’ve identified the point of divergence where these functional oropharyngeal problems originate, our next step will be to understand the vocabulary these cells use to communicate with each other,” LaMantia said.
This research was funded in part by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, part of the National Institutes of Health.
LaMantia is also a professor in the College of Science Department of Biological Sciences and in the Virginia Tech Carilion School of Medicine Department of Pediatrics.




