VTCRI scientists identify new target for developing precision treatment in malignant brain tumors
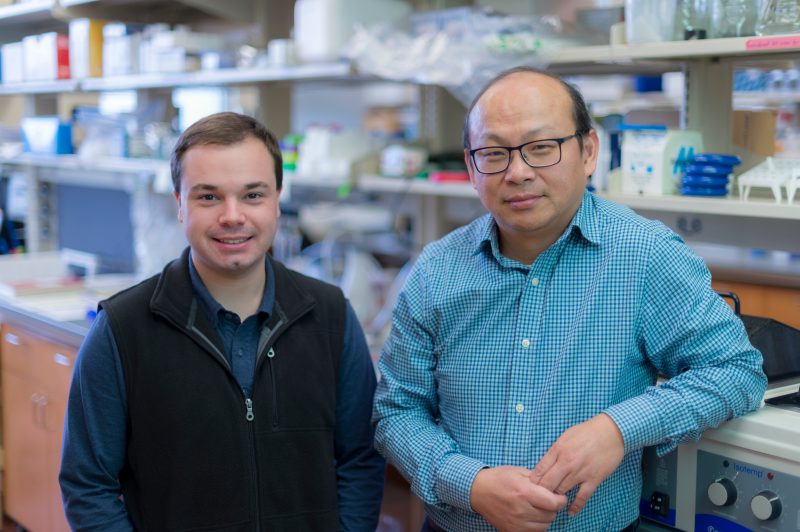
Kevin Pridham (left), a doctoral student in Virginia Tech's Translational Biology, Medicine, and Health graduate program, and Zhi Sheng, an assistant professor at the Virginia Tech Carilion Research Institute, stand in Sheng's laboratory.
A Virginia Tech Carilion Research Institute team has identified a new therapeutic target to treat glioblastoma, the most devastating and common form of brain cancer.
The disease most recently made national headlines last year when Sen. John McCain of Arizona announced his glioblastoma diagnosis in July. Before that, Sen. Ted Kennedy, of Massachusetts, and former Vice President Joe Biden’s son, Beau Biden, both died after battling against glioblastoma.
The scientists published their results in Neuro-Oncology and further contextualized their work in a review paper published in Frontiers in Oncology.
“Patients with glioblastoma survive for less than 15 months from diagnosis on average, even following brain surgery to remove the tumor, radiation therapy, and chemotherapy,” said Zhi Sheng, an assistant professor at the VTCRI and senior author on both papers. “More than 90 percent of the patients who survive more than two years after their first treatments develop tumor recurrence. Unfortunately, these patients are often not eligible for a second brain surgery, and the recurrent tumors become resistant to chemotherapy and radiation.”
Currently, no standard of care exists to prevent or treat recurrent malignant primary brain tumors in patients.
“It is imperative to find effective treatments for recurrent glioblastoma,” said Sheng, who is also an assistant professor of biomedical sciences and pathobiology at the Virginia-Maryland College of Veterinary Medicine.
Sheng and his team previously identified 20 genes that are important for glioblastoma cells to persist. From those genes, they found a particular class responsible for coding proteins that regulate how cellular signaling pathways transmit external messages into the cells. The level of these proteins can be used as biomarkers for predicting the occurrence and prognosis of recurrent glioblastoma.
“Our research demonstrates that patients with glioblastoma who have a greater chance of tumor recurrence often express this class of genes and proteins at high levels,” Sheng said.
Patients could potentially have their protein levels screened to help predict their risk for recurrent glioblastoma. The protein not only indicates risk for recurrent tumors, but scientists can also target it to potentially treat or even prevent subsequent tumors.
Sheng and his team found that a subunit of this gene class, named PIK3C-beta, along with a protein product called p110-beta, are critical for glioblastoma cell survival. The researchers used a molecule to inhibit the expression of this particular protein, stopping p110-beta from communicating necessary information downstream. Without the signals emanating from this protein, the cancer cells started to die off.
“By selectively targeting PIK3C-beta/p110-beta, we were able to suppress the viability and growth of glioblastoma cells in a mouse model,” said Kevin Pridham, a doctoral student in Virginia Tech’s translational biology, medicine, and health graduate program. Pridham, who is conducting his dissertation research in Sheng’s laboratory, was first author on both papers.
According to Pridham, inhibiting the protein not only reduced the survival of glioblastoma cells, it also proved less toxic than traditional chemotherapy to healthy brain cells.
“The chemical inhibitor of PIK3C-beta/p110-beta proved modestly effective by itself,” Pridham said. “Next, we need to test the effect of the inhibitor in combination with other therapies, such as chemotherapy and radiation.”
By further developing this approach, researchers could theoretically design a precise treatment for a person with elevated levels of PIK3C-beta/p110-beta, in conjunction with more traditional treatments such as chemotherapy and radiation.
“Precision medicine is the future for treating patients with glioblastoma,” Sheng said. “The research presented in these papers sets a preclinical stage for future development of precise treatment for patients with a higher chance of tumor recurrence.”
Scientists need to completely understand the full range of variables that influence glioblastoma development, including patient factors such as tumor stage, to more precisely develop this therapeutic strategy. But it’s a step forward, according to Sheng.
“This approach offers hope for a strategy that may be able to improve the prognosis and quality of life for glioblastoma patients,” Sheng said.
This research was supported by the Elsa U. Pardee Foundation and VTCRI.
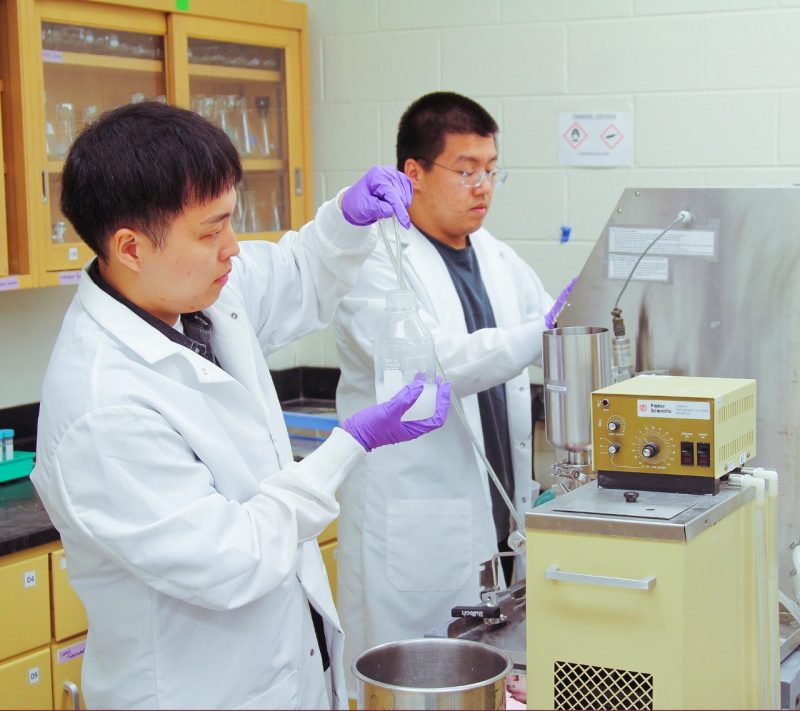
Other contributors to the papers include Lamvy Le, a Virginia Tech Carilion School of Medicine student conducting research in Sheng’s laboratory; Sujuan Guo, a research associate in Sheng’s laboratory; Robin Varghese, a postdoctoral fellow in Sheng’s laboratory at the time of the research; Sarah Algino, an undergraduate researcher in Sheng’s laboratory; Yanping Liang, a research assistant at the VTCRI; Renee Fajardin, an undergraduate researcher in Sheng’s laboratory; Cara Rodgers, a neurosurgeon at Carilion Clinic; Gary Simonds, the chief of neurosurgery at Carilion Clinic; and Deborah Kelly, an associate professor at the VTCRI and in the department of biological sciences in Virginia Tech’s College of Science.