Researchers find way to make resistant brain cancer cells sensitive to treatment
Scientists from the Virginia Tech Carilion Research Institute and clinicians from Carilion Clinic have discovered how to sensitize drug-resistant human glioblastoma cells to chemotherapy.
They published their results in Cancer Research, the scientific journal of the American Association of Cancer Research.
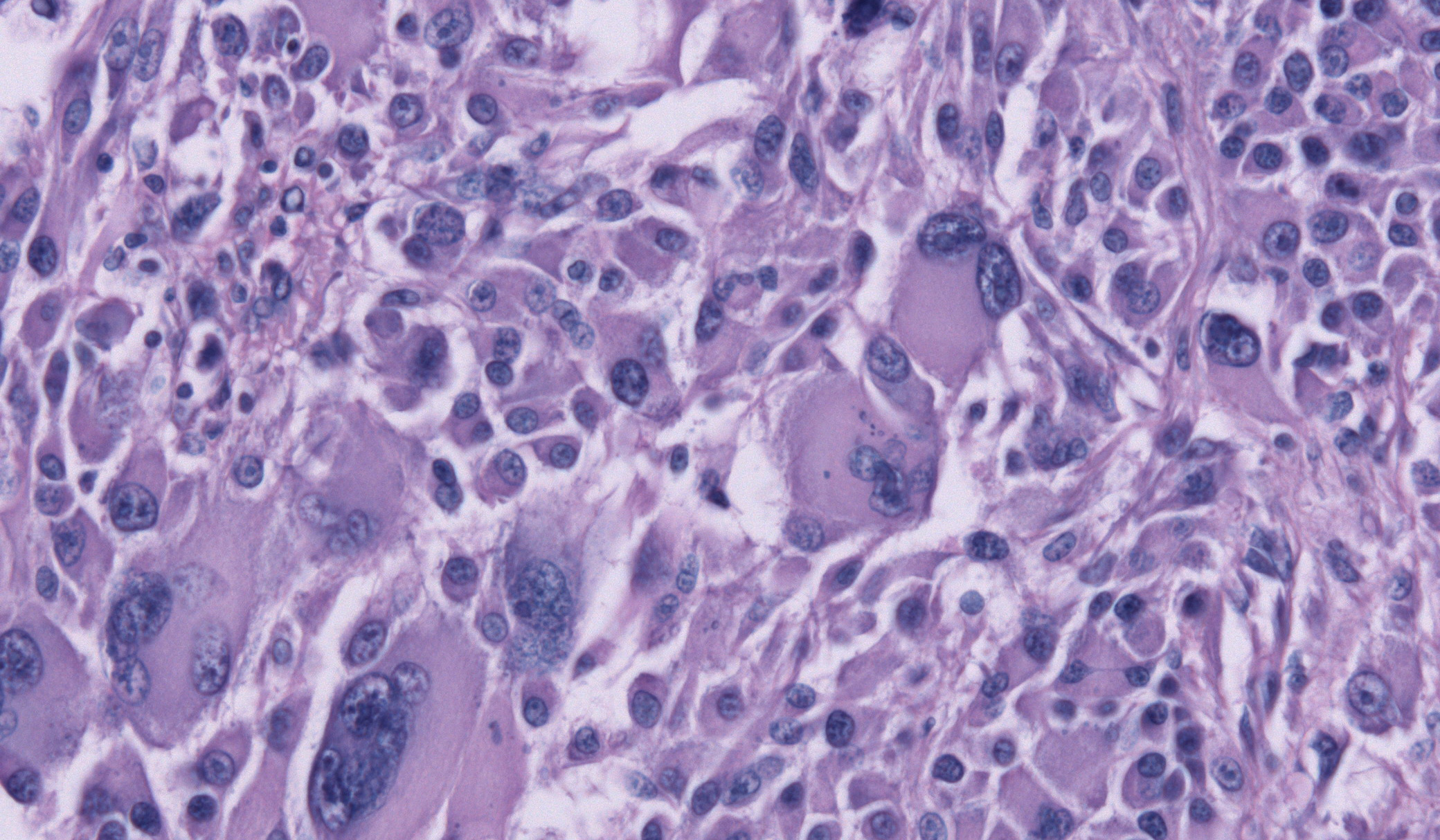
Glioblastoma accounts for almost half of all brain cancers. Fewer than one in 20 patients survive five years after their diagnosis, and treatment involves surgical removal of the cancerous tissue, followed by chemotherapy.
The treatment, although aggressive, typically improves a patient’s survival rate from 12 months to only 14 and a half months. The cancer was recently in the news as the cause of death for Beau Biden, the son of U.S. Vice President Joe Biden.
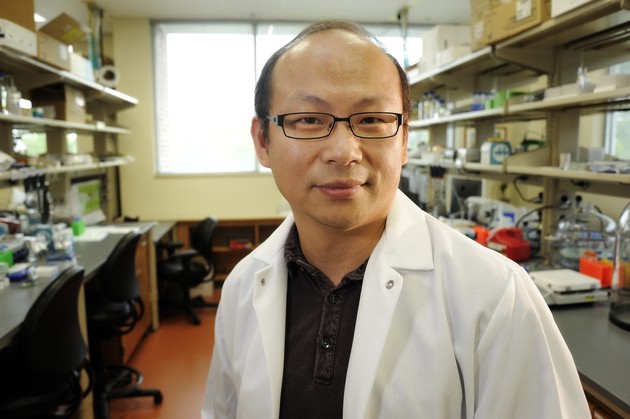
“The grim fact that an increase of only two and a half months represents a significant improvement in survival for glioblastoma patients highlights the urgent need for better treatments,” said Zhi Sheng, an assistant professor at the Virginia Tech Carilion Research Institute and co-corresponding author of the paper.
Patients with gliobastoma often develop a resistance to the principal chemotherapy agent, temozolomide. Known as TMZ, the drug targets quickly replicating cancer cells and lethally damages their DNA, causing the cancer cells to destroy themselves.
“It’s an effective treatment, until it’s not,” said Robert Gourdie, director of the Virginia Tech Carilion Research Institute’s Center for Heart and Regenerative Medicine Research and co-corresponding author on this study. “Glioblastoma cells quickly become resistant, and the treatment stops working. We’ve known for years that this happens, and only now are we beginning to understand why.”
The scientists found that, compared to healthy brain cells, human glioblastoma cells have six to 14 times the amount of a protein called connexin 43.
“The higher the connexin 43 levels, the quicker the cancer cells become resistant to TMZ,” said Gourdie, who is also a professor at the Virginia Tech–Wake Forest School of Biomedical Engineering and Sciences.
Gourdie first encountered connexin 43 while doing heart research. Connexin 43 facilitates cell signaling, but signaling can become overactive in cells damaged by trauma or disease.
Gourdie and his research team developed a peptide called aCT1 (pronounced act one) to inhibit connexin 43-caused overactivity. The result was damaged tissue healed more quickly, with lower amounts of inflammation and scarring.
The researchers formed a company, FirstString Research Inc., to further develop the peptide as a treatment for chronic, slow-healing wounds, such as diabetic foot ulcers and venous leg ulcers. The peptide has since progressed through two clinical trials, and none of the 300 people treated with aCT1 suffered an adverse reaction.
“Connexin 43 is prevented from opening more communication channels in the damaged cell, allowing the wound to heal more quickly,” Gourdie said.
The scientists wondered whether the same inhibition of connexin 43 would allow cancer cells that had grown resistant to TMZ to recover their sensitivity to the drug. So the researchers administered a combination treatment of aCT1 and TMZ to human glioblastoma cells surgically obtained by neurosurgeon Gary Simonds and his team at Carilion Clinic.
“In every instance, the cells began to respond to TMZ again,” said Sheng, who is also an assistant professor of biomedical sciences and pathobiology at the Virginia–Maryland College of Veterinary Medicine. “The combination of aCT1 and TMZ caused a striking recovery in sensitivity to the treatment.”
Not only were the tumor cells resensitized to the combined TMZ treatment, but so were the individual cancerous stem cells. Glioblastoma stem cells are particularly dangerous for patients, because they migrate in the brain and hide from the surgeon’s scalpel.
The mechanism by which aCT1 and TMZ induce sensitization remains a mystery, though.
“Our laboratory teams and collaborative partners at Carilion Clinic are continuing to study exactly how the combination treatment works,” said Gourdie. “We suspect the signaling pathways are altered, and we hope our continued research will elucidate the mechanism.”
Alonzo Ross, a professor emeritus in the Department of Biochemistry and Molecular Pharmacology at the University of Massachusetts Medical School, said he is enthusiastic about the work and its potential for clinical translation. Ross, who conducts glioblastoma research, was not involved in this study.
“TMZ enhances survival but does not cure glioblastoma,” Ross said. “These researchers have taken the logical approach of combining TMZ with a second drug to improve its potency. Although there’s still much work to do before this method can be applied in the clinic, I have high expectations that this work will eventually help glioblastoma patients.”
The researchers believe their work could apply to other tumor types, as well. TMZ is often used as a chemotherapy agent for several other cancers, including breast and lung cancers, which can spread in the brain and become resistant to the drug.
“Administering aCT1 with TMZ could provide a powerful new therapy for glioblastoma and other cancers,” Sheng said. “A National Institutes of Health–supported, basic science study of how cells talk to each other led to a potential treatment for the deadliest brain cancer, and it might aid in treating several other cancers. That’s science.”