Scientists visualize potential brain cancer treatments in real time
Virginia Tech Carilion Research Institute scientists have developed new imaging techniques to watch dangerous brain tumor cells respond to treatment in real time.
Published in NANO Letters, the study was led by Zhi Sheng and Deborah Kelly, both assistant professors at the institute, and describes how the research team used nanotechnology to watch tumor stem cells respond to therapy.
“We’ve never been able to directly observe the actions of potential cancer treatments this way before,” said Sheng, a cancer biologist and an assistant professor of biomedical sciences and pathobiology at the Virginia–Maryland College of Veterinary Medicine. “It was astounding. In all my years of researching glioblastoma, I had seen only static images.”
Both Sheng and Kelly credit Elliot Pohlmann, a fourth-year Virginia Tech School of Medicine student and the paper’s first author, for sparking the collaboration between their laboratories on this particular project.
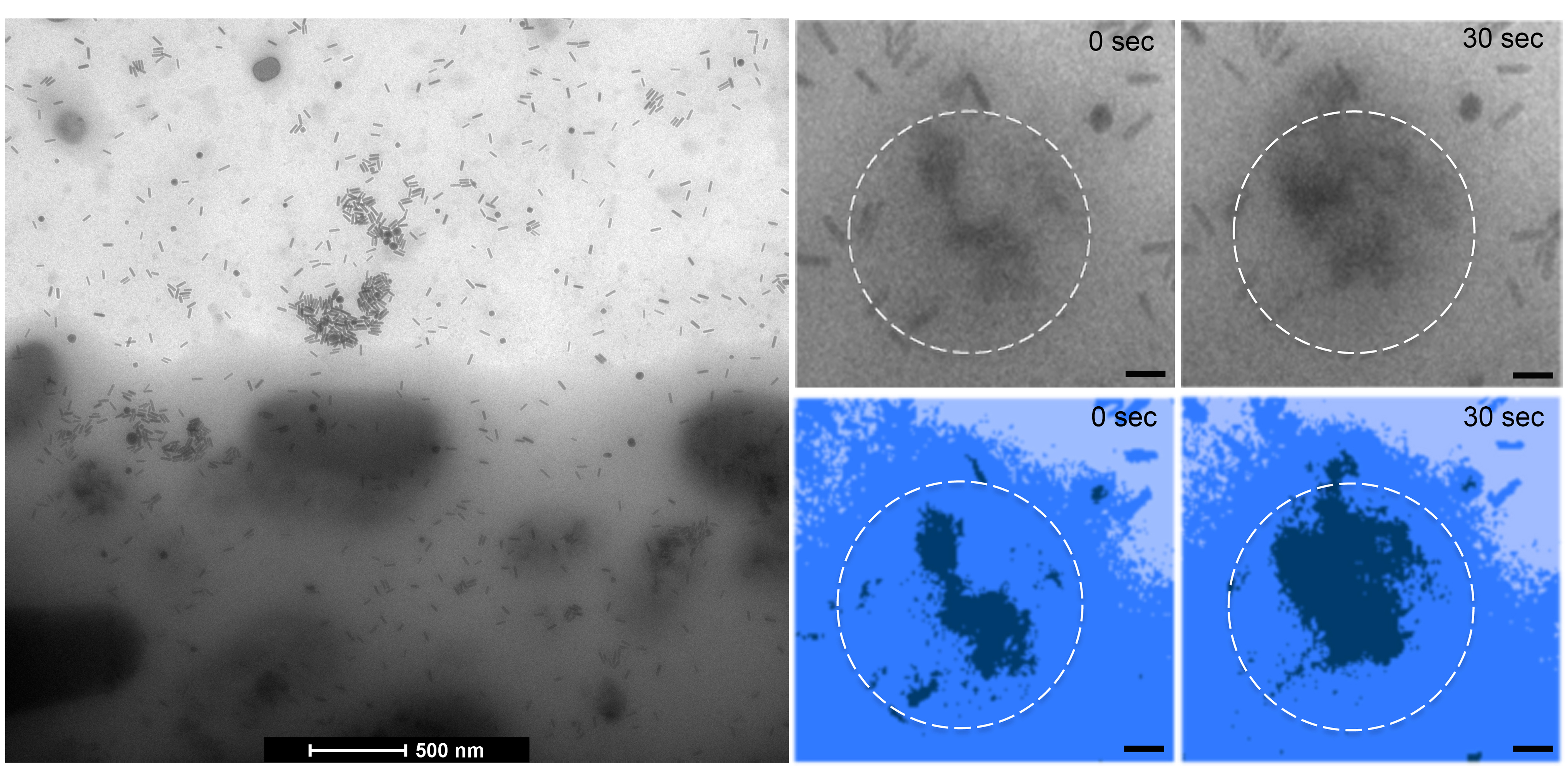
“We realized that glioblastoma stem cells could work very well with the imaging techniques Dr. Kelly was developing,” Pohlmann said. “With a little trial and error, we’ve produced visually striking images.”
Glioblastoma is a brain cancer with a poor prognosis. Even with surgical interventions or traditional treatments, some of the cells – the stem cells – tend to survive and grow new tumors.
“Glioblastoma tumors are hard to target,” Sheng said. “They’re aggressive and resistant to therapeutics. With our imaging techniques, we may be able to gain new insights into how the cells dynamically respond to treatments.”
The research team separated the hard-to-kill stem cells from the general glioblastoma population by attracting the stem cells to a microchip coated with antibodies. The scientists then used a specially designed microfluidic chamber to trap the cells in a liquid environment.
Once the samples were in place, the scientists blasted them with gold nanorods – similar to what is used in some cancer treatments – and watched the process in cell cultures using in situ transmission electron microscopy.
Kelly partnered with coauthor Madeline Dukes, an applications scientist at Protochips Inc., to develop the microfluidic equipment.
“We were curious to see whether we could isolate these types of toxic cells from the other brain tumor cells, while developing new imaging tools at the single-cell level to visualize the course of therapies needed to eradicate these cells,” said Kelly, the project’s lead scientist and a biophysicist with extensive expertise in high-resolution imaging. She is also an assistant professor of biological sciences in Virginia Tech’s College of Science.
“It’s exciting to see things no one else has seen before,” Pohlmann said. “It’s even more exciting to produce the profound images with this project.”
Researchers say the technology has many potential applications.
“One may be able to directly observe an influenza virus, HIV, or other human pathogens infecting a cell, or even test new cancer treatments at the cellular level,” Kelly said.
Sheng pointed to another characteristic that makes cancer cells difficult to treat: broad heterogeneity. In the same cancer population, even neighboring cells can differ drastically, and each cell can respond to treatments differently.
“We can look at single-cell delivery of cancer treatments, and see how the individual cells respond,” Sheng said. “If we can learn how to kill these cells, we should be able to improve our chances of developing effective treatments by being able to directly observe the effects of the possible therapeutics.”
Kelly and Sheng, whose offices are on the same floor of the Virginia Tech Carilion Research Institute in Roanoke have worked together previously and are also currently working on understanding the mechanisms underlying hereditary breast cancer.
Written by Ashley WennersHerron.




