Virginia-Maryland Regional College of Veterinary Medicine researcher says banned pregnancy drug impacts fetal immune system
A synthetic estrogen—diethylstilbestrol (DES)—prescribed to women in the 1940s, 1950s, and 1960s to prevent miscarriages had serious, untoward effects in daughters of these women, including the development of a rare type of cancer of the uterus. There has been renewed interest in light of an Oct. 6 report in the New England Journal of Medicine documenting lifelong health complications facing daughters of women given DES.
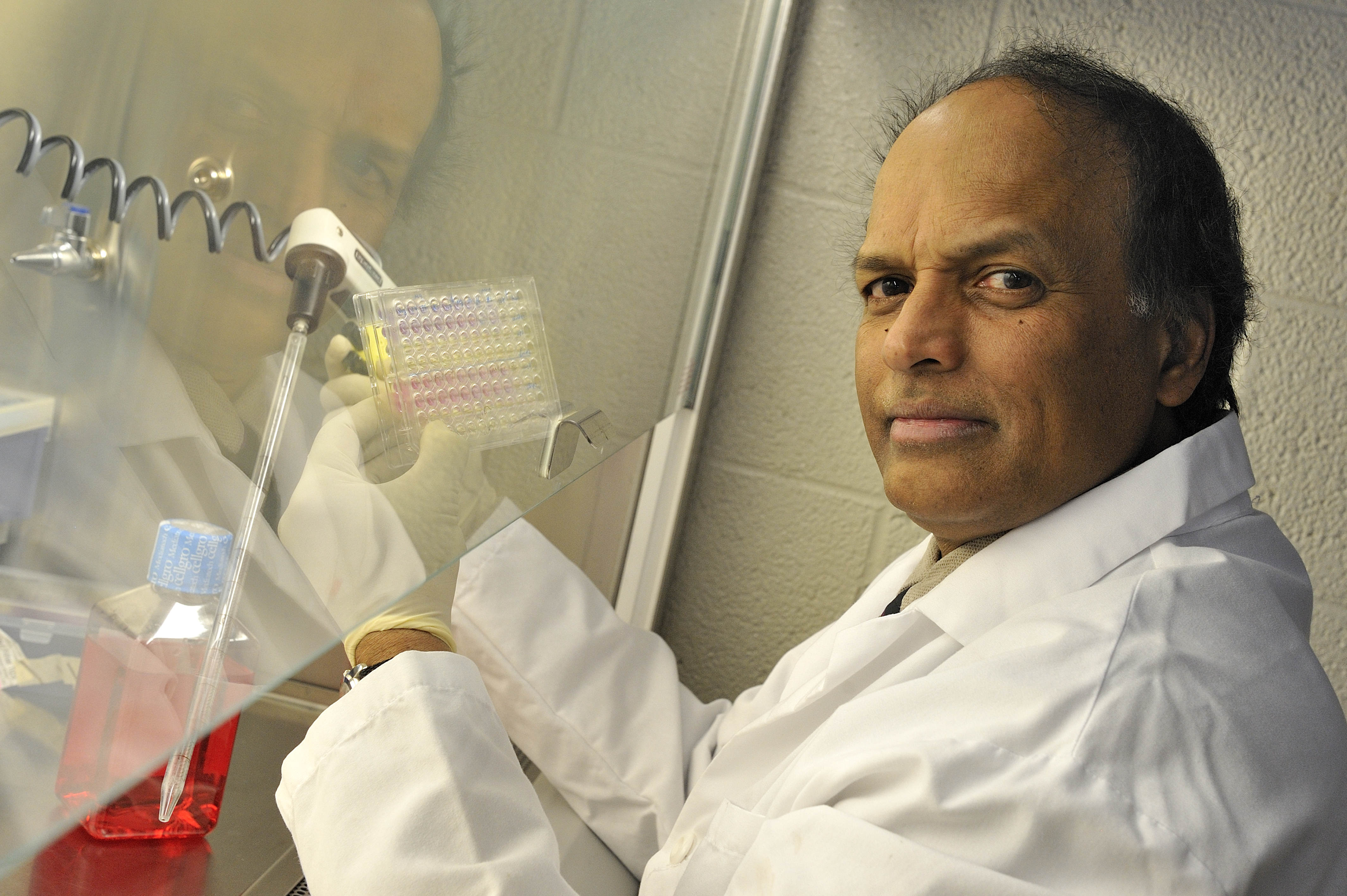
Reproductive tissues are not the only targets of DES. The immune system is also known to be a target for estrogens. Dr. S. Ansar Ahmed, professor of immunology in the Virginia-Maryland Regional College of Veterinary Medicine at Virginia Tech, led a National Institutes of Health (NIH) study in the 1990s on how exposure to DES in utero affects the immune system later in life using a mouse model.
“We decided to look at how giving DES to mothers changes the immune system after birth,” said Ahmed, who is also head of the Department of Biomedical Sciences and Pathobiology. “Exposure to hormones such as DES can create a different environment for the fetal immune system. This is a very sensitive time in the ‘education’ of the immune system. Exposure of the fetus to DES during this sensitive time can interfere with this ‘education’ of the immune system.”
According to Ahmed, many disorders resulting from prenatal exposure to DES become evident after puberty and maturity. This suggested to Ahmed and his colleagues that individuals exposed to DES prenatally might have a “deviant or more sensitive” response to their own sex hormones at maturity.
The recent New England Journal of Medicine report found that women whose mothers took DES have significantly higher rates of a number of reproductive problems, including infertility, miscarriage, and premature births. There are more than 2 million women in the United States who were exposed to DES in utero.
The U.S. Food and Drug Administration banned pregnant women from using the drug after a 1971 study found that it caused a rare vaginal tumor in girls and women exposed to it.
Because of the complexity of researching the effects of synthetic estrogens on the immune system, Ahmed turned his attention to the role of natural estrogen and other immunomodulators on transcription factors and gene activation events after completing the NIH study.
Today, he also conducts research on inflammatory cytokine signaling in mouse models and microRNA (miRNA) regulation of the immune system in health and disease.
In 2010, Ahmed and his colleagues identified common miRNAs present in three strains of autoimmune-prone mice, likely revealing where the breakdown in the body’s lymphocyte molecular regulatory machinery takes place. This could potentially impact future diagnosis and treatment of lupus, a chronic autoimmune disease which affects more than 5 million people worldwide.
The veterinary college’s research program ranges from basic, molecular research to translational medicine and includes public health and infectious disease control in addition to companion animal care. Last September, the college broke ground on a new Infectious Disease Research Facility, slated for completion later this year.




